Abstract
Background
Patients (Pts) with myelodysplastic syndrome (MDS) are at a high risk for increasingly resistant and severe infections. Predisposing factors include neutropenia and functional impairment of neutrophils and lymphocytes, secondary iron overload, chemotherapy toxicity and history of severe infections. The Infectious Diseases Society of America has classified commonly resistant bacteria as ESKAPE (Enterococcus, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter, Pseudomonas aeruginosa, Enterobacter). Other difficult-to-treat infections such as Enterobacteriaceae organisms (E. coli, Proteus) and Clostridium difficile can be added to this group (changing the acronym from ESKAPE to ESCAPE). As part of the HONORS award grant from the American Society of Hematology (ASH), we are presenting a subset analysis in MDS.
Methods
We performed a retrospective review of the rate of ESCAPE infections, resistance profile, and outcomes in pts with myelodysplastic syndrome at the Houston Methodist Hospital from 2006 to 2015.
The pt information was obtained by data mining from METEOR (Methodist Environment for Translational Enhancement and Outcomes Research), a clinical data warehouse with over 3 million pts and over 10 million unique patient encounters. We queried for MDS along with hospitalizations due to bacterial infections using ICD-code 9 and 10. Baseline demographics and overall outcomes were obtained. Analysis with unpaired t-test for elevated ferritin levels and leukopenia was also done.
Results
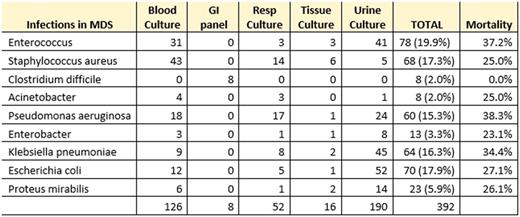
Out of the 234 pts with MDS, 566 infectious events were identified; 69% were ESCAPE infections. Median age was 77 years old and male to female ratio was 1.17.
The bacteria most frequently isolated were Enterococcus (19.9%), E. coli (17.9%) and Staphylococcus aureus (17.3%). C. difficile and Acinetobacter had the lowest frequency of infection (2%). Cultures were isolated predominantly from urine (48.5%) and blood (31.6%). The frequency of infections in pts with elevated ferritin was almost 50%. Leukopenia (49%) and neutropenia (33%) were also recorded. Median ferritin level was 898 and median WBC was 2.11. Unpaired T-test did not show any statistical difference between ESKAPE and not-ESKAPE events for elevated ferritin or leukopenia, however; using the F-test a statistical difference in variance was found for high ferritin between the groups.
A prevalent resistance to levofloxacin was detected in most gram-positive and gram-negative organisms (39-53%). Pseudomonas, E. coli, Enterobacter and Klebsiella showed a significant resistance to broad-spectrum antibiotics including aztreonam (23%-36%) and cefepime (22%-33%). Frequency of resistance to piperacillin-Tazobactam and imipinem was less than 20% in almost all organisms. Vancomycin was the most used antibiotic (86.2%), followed by cefepime (42.4%).
Pseudomonas aeruginosa had the highest mortality (38.3%), followed by Enterococcus (37.2%) and Klebsiella pneumoniae (34.4%).
Conclusions
ESCAPE infections are frequent in MDS pts. Enterococcus is the most predominant organism but gram-negative infection rate is also high. ESCAPE Infections seem to be more common in pts with elevated ferritin levels although it was not statistically significant using two tailed t test. Gram negative pathogens had an increased resistance to broad-spectrum antibiotics and higher mortality rates overall. A disturbing trend towards levofloxacin resistance, a prophylactic antibiotic, was also noted in all bacteria, therefore changes and new strategies for preventing highly resistant infections by ESCAPE organisms are needed.
IPSS data and further statistical review will be presented at the ASH Meeting, Georgia 2017.
Gentille Sanchez: ASH: Research Funding. Iyer: Takeda: Research Funding; Genentech: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal